Occipital Neuralgia symptoms and Treatment
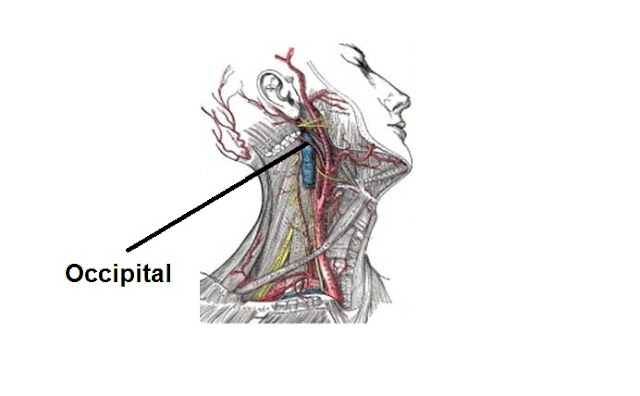
Occipital Neuralgia is a condition in which the occipital nerves, the nerves that run through the scalp, are injured or inflamed. This causes headaches that feel like severe piercing, throbbing or shock-like pain in the upper neck, back of the head or behind the ears. and this is not whiplash injury.
Causes
Occipital neuralgia can be the result of pinched nerves or muscle tightness in the neck. It can also be caused by a head or neck injury. Occipital neuralgia can either be primary or secondary. A secondary condition is associated with an underlying disease.
Although any of the following may be causes of occipital neuralgia, many cases can be attributed to chronic neck tension or unknown origins.
- Osteoarthritis of the upper cervical spine
- Trauma to the greater and/or lesser occipital nerves
- Compression of the greater and/or lesser occipital nerves or C2 and/or C3 nerve roots from degenerative cervical spine changes
- Cervical disc disease
- Tumors affecting the C2 and C3 nerve roots
- Gout
- Diabetes
- Blood vessel inflammation
- Infection
Symptoms
Symptoms of occipital neuralgia include continuous aching, burning and throbbing, with intermittent shocking or shooting pain that generally starts at the base of the head and goes to the scalp on one or both sides of the head. Patients often have pain behind the eye of the affected side of the head. Additionally, a movement as light as brushing hair may trigger pain. The pain is often described as migraine-like and some patients may also experience symptoms common to migraines and cluster headaches.
When & How to Seek Medical Care
Occipital neuralgia can be very difficult to diagnose because of its similarities with migraines and other headache disorders. Therefore, it is important to seek medical care when you begin feeling unusual, sharp pain in the neck or scalp and the pain is not accompanied by nausea or light sensitivity. Begin by addressing the problem with your primary care physician. They may refer you to a specialist.
Testing & Diagnosis
Diagnosis of occipital neuralgia is tricky, because there is not one concrete test that will reveal a positive or negative diagnosis. Typically, a physical examination and neurological exam will be done to look for abnormalities. If the physical and neurological exams are inconclusive, a doctor may order further imaging to rule out any other possible causes of the pain. A magnetic resonance imaging (MRI) test may be ordered, which can show three-dimensional images of certain body structures and can reveal any impingement. A computed tomography scan (CT or CAT scan) will show the shape and size of body structures. Some doctors may use occipital nerve blocks to confirm their diagnosis.
Treatment
Treatment of occipital neuralgia aims to alleviate the pain; however, it is not a cure. Interventions can be surgical or non-surgical.
Non-surgical Treatments
- Heat: patients often feel relief when heating pads or devices are placed in the location of the pain. Such heating pads can be bought over-the-counter or online.
- Physical therapy or massage therapy.
- Oral Medication:
- Anti-inflammatory medications;
- Muscle relaxants; and
- Anticonvulsant medications.
- Percutaneous nerve blocks: these injections can be used both to diagnose and treat occipital neuralgia.
- Botulinum Toxin (Botox) Injections: Botox injections can be used to decrease inflammation of the nerve
Surgery
Occipital Nerve Stimulation: This surgical treatment involves the placement of electrodes under the skin near the occipital nerves. The procedure works the same way as spinal cord stimulation and uses the same device. The procedure is minimally invasive and surrounding nerves and structures are not damaged by the stimulation. It is an off-label indication for an FDA-approved device.
Spinal Cord Stimulation: this surgical treatment involves the placement of stimulating electrodes between the spinal cord and the vertebrae. The device produces electrical impulses to block pain messages from the spinal cord to the brain.
C2,3 Ganglionectomy- This treatment involves the disruption of the second and third cervical sensory dorsal root ganglion. Acar et al (2008) studied the short-term and long-term effects of this procedure. The study found that 95% of patients had immediate relief with 60% maintaining relief past one year.
Follow-up
Patients are encouraged to regularly follow up with their primary care providers and specialists to maintain their treatment. Surgeons like patients to return to the clinic every few months in the year following the surgery. In these visits, they may adjust the stimulation settings and assess the patient’s recovery from surgery. Following up with a doctor ensures that the patient is getting correct and effective care. Patients who undergo occipital nerve stimulation will follow up with a device representative who will adjust their device settings and parameters as needed, alongside their doctors.
The AANS does not endorse any treatments, procedures, products or physicians referenced in these patient fact sheets. This information provided is an educational service and is not intended to serve as medical advice. Anyone seeking specific neurosurgical advice or assistance should consult his or her neurosurgeon, or locate one in your area through the AANS’ Find a Board-certified Neurosurgeon online tool.